This article was developed as a part of assignments during my education in 2013. For citation purpose, please use: Gunawan, J. (2013). The Innovation of Nursing Care Delivery System: A Hybrid Model. Retrieved from jokogunawan.com.
Download free PDF.
Background
Care delivery systems are conceptual or philosophical frameworks that describe how organizations approach the care delivered to their patients. It is important to identify the nursing concepts that keep care delivery focused on the patient and their family. The organization of care delivery is determined by a variety of factors such as economic issues, leadership beliefs, and the ability to recruit and retain staff. Ideally, evidence of the effect of care models on quality care would also be a major factor in decision making.
Historically, four traditional care models have dominated the organization of inpatient nursing care, such as total patient care, functioning nursing, team nursing, and primary nursing. Despite the interest in a variety of care models, it is difficult to discern which models work best, whether the traditional or the nontraditional inpatient nursing care models. When we discuss about model of care we are essentially talking about nursing issues: increasing nursing shortage, the number of new nurses, different background of nurses, the number of staff, and cost of delivery model. Many nursing departments have reported the implementation of innovative nursing models. However, it lacks of evidence of innovation model to face those issues.
In this paper, the authors provide information, which basically nurses need to understand the positive and negative consequences of each model in order to plan and propose to decision- makers the most efficient and effective way to deliver care. Nurses need to understand the different models of care so that we can make a good case for one model or the other, or a hybrid of several. The authors propose that a hybrid model is a combination between two or more models which will be appropriate to answer the nursing issue, especially in hospital- inpatient setting.
The paper aimed
- To describe the concept of patient care delivery model
- To describe the diffusion process of hybrid model in inpatient setting
Concept of Patient Care Delivery Model
Total patient care/Case Method
In this model, the RN is responsible for all of the care provided to a patient for a shift. It is the oldest nursing care delivery model. This is the way most nursing students were taught – take one patient and care for all of their needs. The consequences of teaching nursing this way was that reality shock hit upon graduation when the new graduate hit the floors and had to care for more than one patient. Even in the case of the student nurse, the students frequently do not provide all of the care as they may not be qualified to do the work. We may still see this model used in critical care areas, labor and delivery, or any area where one nurse cares for one patient’s total needs. It is interesting to note that nurses were self- employed when the case method came into being, because we were primarily practicing in homes. Home health agencies use a form of this model when nurses are assigned patients and provide all home care. Even this has been adapted; as the RN may delegate or coordinate some of the care to a home care aide or other service such as physical therapy or dietician for example.
| Advantages: | RNs were self-employed. Patient needs were quickly met Close relationship between the RN and the patient |
| Disadvantages: | Cost! RNs are expensive |
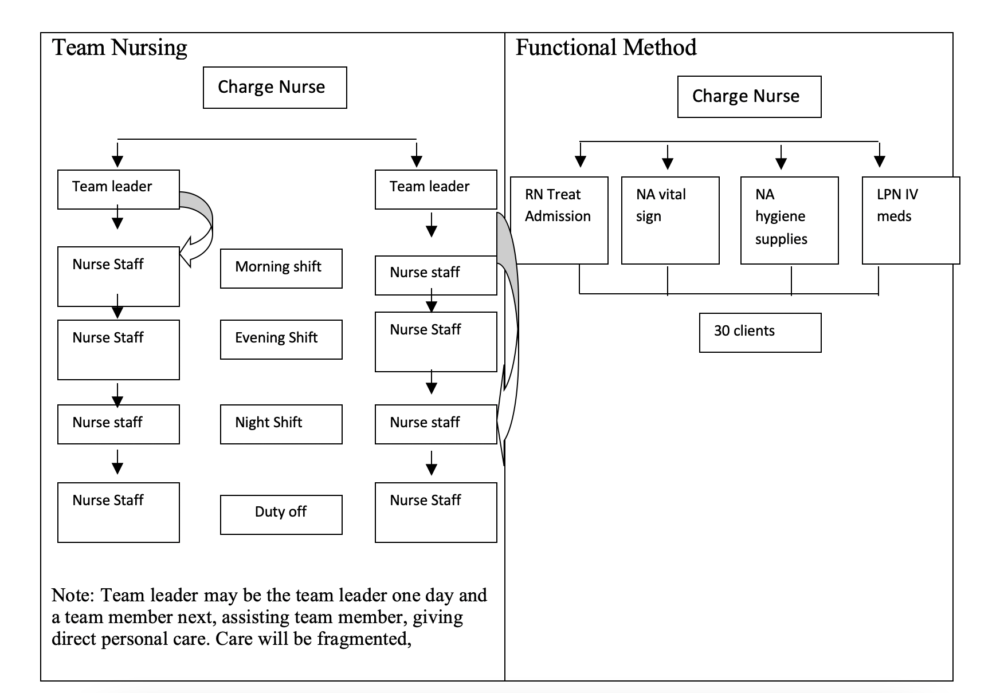
Functional Nursing
This model is also referred to as the Task Method, and for good reason! Functional nursing evolved during the Depression when RNs went from being private practitioners (see above) to becoming employees for the purposes of job security. Once WWII broke out, however, nurses left to care for the soldiers which left the hospitals short-staffed. To accommodate this shortage, hospitals increased their use of ancillary personnel (sound familiar?). For efficiency, nursing was essentially divided into tasks, a model that proved very beneficial when staffing was poor. The key idea was for nurses to be assigned to TASKS, not to patients. For example, one nurse would be responsible for all the treatments, another nurse for all the medications, and so on.
| Advantages: | A very efficient way to delivery care. Could accomplish a lot of tasks in a small amount of time. Staff did what only they were capable to do: no extraneous work was added that could be done by assistive personnel. |
| Disadvantages: | Care of persons became fragmented. Patients did not have one identifiable nurse and the nurse had no accountability. Very narrow scope of practice for RNs. Lead to patient and nurse dissatisfaction |
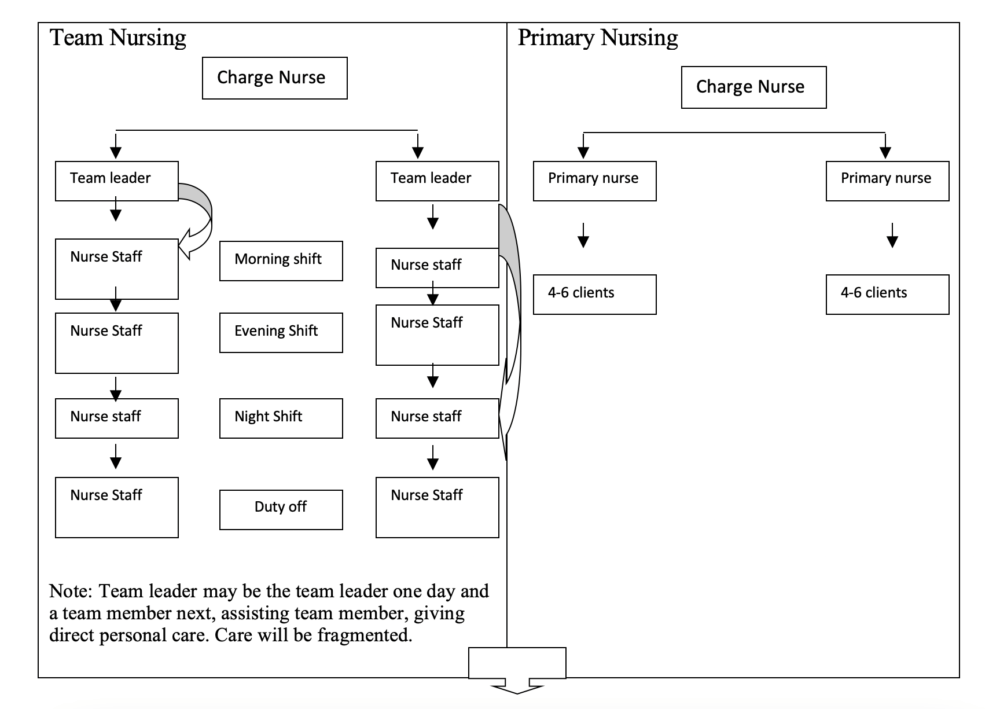
Team Nursing
This is the most commonly used model and is still in use today. It was developed in the 1950’s after WWII when there was a severe nursing shortage and major changes in technology (replaced functional nursing) and to somewhat ameliorate the fragmentation that was inherent in the functional model (see above). In the past, approaches to team nursing was thought to use the decentralized decision making with decisions made closer to the patient, there actually was limited team member collaboration. These teams tended to communicate only among themselves and not as well with physicians. Today, the goal of the Team method is for a team to work democratically. In the ideal team, an RN is assigned as a Team Leader for a group of patients. The Team Leader has a cadre of staff reporting to her and together they work to disseminate the care activities. The team member possessing the skill needed by the individual patient is assigned to that patient, but the Team Leader still has accountability for all of the care. Team conferences occur in which the expertise of every staff member is used to plan the care; a hallmark is that each member’s input (RN, LPN, NA, etc) is considered essential for the process to work. As is obvious, the Team Leader must be both a skilled clinician and an effective group leader.
| Advantages: | Each member’s capabilities are maximized so job satisfaction should be high. Patients have one nurse (the Team Leader) with access to other providers |
| Disadvantages: | Requires a team spirit and commitment to succeed RN may be the Team Leader one day and a team member the next, thus continuity of patient care may suffer. Care is still fragmented with only 8 or 12 hour accountability. |
Primary Nursing
Primary nursing was developed in the 1980’s by Marie Manthey and the hallmark of this model is that one nurse cares for one group of patients with 24 hour accountability for planning their care. In other words, a Primary Nurse (PN) cares for her primary patients every time she works and for as long as the patient remains on her unit. An Associate Nurse cares for the patient in the PN’s absence and follows the PN’s individualized plan of care. This is a decentralized delivery model: more responsibility and authority is placed with each staff nurse. It has been debated whether PN is a cost-effective model. Some say it is because the RN has all the skills necessary to move the patient through the health care system quickly. Others say it is not cost effective because RNs spend time doing things that other, less expensive employees can do.
| Advantages: | Increased satisfaction for patients and nurses. More professional system: RN plans and communicates with all disciplines. RNs are seen as more knowledgeable and responsible. RNs more satisfied because they continue to learn as a function of the in-depth care they are required to deliver. |
| Disadvantages: | Intimidating for new graduates who are less skilled and knowledgeable. Where do we get all these RNS during times of shortage? |
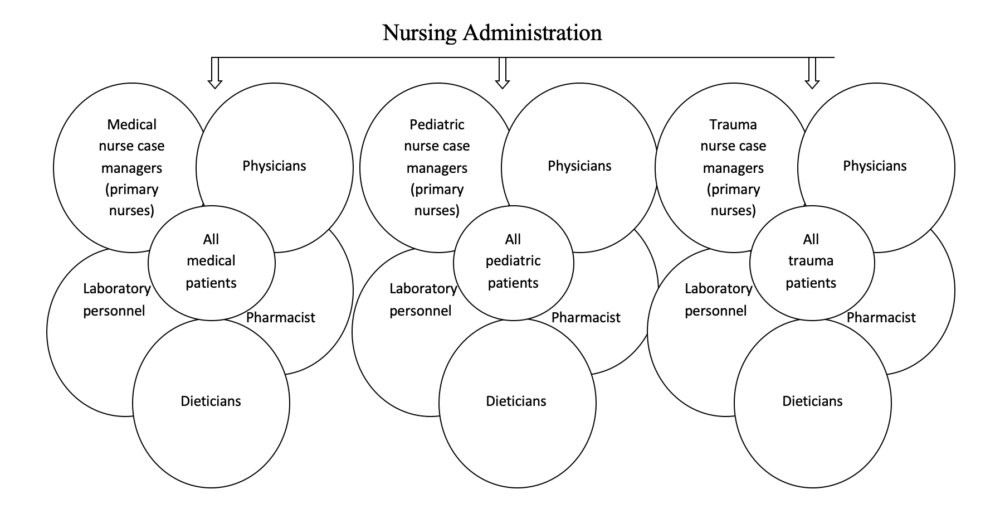
Case Management
Case management is a collaborative process that assesses plans, implements, coordinates, monitors and evaluates options and services to meet an individual’s health needs through communication and available resources to promote quality, cost-effective outcomes. In case management, nurses address each patient individually, identifying the most cost-effective providers, treatments and case settings possible. Case management often manages care using critical pathways and multidisciplinary action plans to plan patient care. Clinical pathways are a strategy for assessing, implementing, and evaluating the cost-effectiveness of patient care. Advantages: they do provide some means of standardizing medical care for patients with similar diagnosis. Some of the results reported since Case Management has become more popular for inpatient nursing care: Length of stay has decreased, RNS and MDS like it, Provides a new marketing potential for hospitals, it increases the chance that agencies can recruit and retain the best and the brightest. Disadvantage: they pose in accounting for and accepting what are often justifiable differentiations between unique patients who have deviated from their pathway.
Kind of Innovation of Care Delivery Models
Clearly, the organizational landscape of health care delivery is being rearranged. Because of facing with the twin challenges of growing demand for expensive acute care and insufficient supply of key health care professionals, leading hospital systems, integrated systems, clinics, and health plans are designing new models to deliver efficient, effective health care. So, that is reasons we need Innovative Care Delivery Models.
At the beginning of 2007, the Robert Wood Johnson Foundation funded an original research project to identify and profile new models of care that could be widely replicated throughout the United States. Based on conversations with health care leaders, Health Workforce Solutions LLC (HWS) developed a set of criteria, listed below, to designate innovative care delivery models. It is nursing care delivery model, or interdisciplinary care delivery models with a nursing component and an acute care interface, including transitional care to home setting. Innovative-models will be considered innovative if they improve caregiver efficiency, quality, and/or cost through one or more of the following changes:
- New roles for nurses and other professionals
- New roles for allied health professionals, students, new graduates
- Use of new technology (or use of technology in a new and novel way)
- Redesign of physical layout, inventory, or other support systems
Model has to demonstrate measurable improvement in quality, safety, cost, and/or (patient or caregiver) satisfaction. It decreases long-term demand for acute care nursing through more effective leveraging of nurses. Model can be replicated in other facilities or communities, and primarily serves adult patients (>18)
So the question is “How to innovation a new Model?” To answer this question, many researchers go to find the result. And they give a common process to innovation a new model, include five steps. Organizations should support processes to facilitate the generation, testing and implementation of new ideas.
STEP 1 – Assess the problem
Organizations should conduct a thorough assessment of the problem or process in need of change. This includes conducting a literature review and internal and external interviews, including discussions with patients and families, to determine the scope of the problem across the industry and how other organizations have addressed it. This stage also should include an assessment of available resources to address the problem.
STEP 2 – Develop a plan
Once the assessment is complete and the scope of the issue is defined, brainstorming new solutions can begin. The information gleaned from the assessment should be used to conduct a risk analysis and to draw up a project plan that outlines the scope of the project, including the goal(s), projected cost, and project champion, description of the problem being addressed and how the innovation will solve the problem.
STEP 3 – Test
This stage involves testing the innovation at the front line and validating its effectiveness. The testing phase should have defined start and end dates.
STEP 4 – Implementation
Too often, organizations invest heavily up front in brainstorming and idea generation and not enough in bringing innovative ideas into practice. Communication is important to create understanding and set expectations up front. An action plan should detail the implementation process, step-by-step.
STEP 5 – Post – Implementation
The implementation process is not the final step in bringing innovation to fruition. It’s important to continually assess and tweak the innovation. This time is also important for assessing ways to spread the innovation to other relevant areas within the organization. One of the most important criteria identified was the ability to replicate the model widely in health care organizations throughout the country. Additional criteria are listed below.
- Innovation, as exemplified by redesigned provider roles and teams, greater reliance on interdisciplinary teams, introduction of new technology, increased responsiveness to patients, and/or the redesign of the physical care environment.
- Sustainability of the model at the original organization and likely sustainability at replication sites.
- Demonstrated impact in terms of reduced cost or utilization, improved patient safety and quality, improved patient and provider satisfaction, and ultimately the ability to reduce the long-term demand for acute care nurses.
The new models of care delivery
The new models are organized into three broad categories of care delivery: acute care, bridging the continuum, and comprehensive care models
- The acute care model provides advanced nursing care across the continuum of health care services to meet the specialized physiologic and psychologic needs of adult patients with complex acute, critical, and chronic health conditions. This care is continuous and comprehensive. The population in acute care practice includes acutely and critically ill patients experiencing episodic illness, exacerbation of chronic illness, or terminal illness. The short-term goals include patient stabilization, minimization of complications, and promotion of physical and psychological well-being. The long-term goal is to restore maximal health potential while evaluating risk factors in achieving this outcome.
- Bridges the continuum model are extending their focus beyond the sponsoring organization’s primary setting of care. For some of these models, hospitals serve as the primary setting of care, but the model follows the patient and her or his care into the home, outpatient clinics, and long-term care facilities. In other cases, an outpatient clinic serves as the primary setting of care, but the model follows the patient into the hospital, home, and long-term care facilities. The non-clinical services and activities help reach individuals who have not been reached effectively by health care professionals. In addition, the activities provide an opportunity for people to come together and discuss health promotion and healthy living.
- Comprehensive care model of delivery is centered on the patient. Advantages of the comprehensive care model are that it identifies one primary care provider for the patient, there is continuity of care, and the chief complaint of the patient is addressed earlier. Therefore, this model is considered the better model for delivery of care both for the clinical training and from the patient care than the traditional model.
Example of an Innovative Model
The primary care team
The primary care team shares the responsibility of providing care for an assigned group of patients. Target of model is general inpatient population. The model has been organization in The Seton Family of Hospitals is a not-for-profit health system with five urban acute care hospitals, two rural hospitals and a mental health hospital. The health system is headquartered in Austin, Texas. The Seton Family of Hospitals has four Magnet-designated hospitals.
The Primary Care Team model grew out of the desire to create a culture of safety in an increasingly difficult care environment where LOS is declining, patient acuity is increasing, and the portion of RN positions filled by novice nurses is increasing. Specifically, Seton developed the Primary Care Team in order to achieve the following goals: (1) Improve quality of care, (2) Improve patient safety, (3) Increase patient, physician and staff satisfaction, (4) Decrease LOS, (5) Reduce or result in no change to costs. Origin and Evolution of the Model is the Primary Care Team model in 2000 by Seton Family of Hospitals nurses. The model grew out of an initiative to design a care delivery model that would retain experienced nurses in an oversight role for all patients, foster team building and mentoring of new nurses, and enable a strong patient partnership. Seton’s participation in the Robert Wood Johnson Foundation initiative Transforming Care at the Bedside helped them continue to make changes to the model and implement it in more units. The PCT model was further strengthened by staff-led innovations.
The center of the Primary Care Team model is the nursing team, which is typically comprised of an experienced RN care manager, an RN or LVN provider and a clinical assistant (CA). The primary care team shares the responsibility of providing care for an assigned group of patients, and each member of the team has a clearly-defined role. The experienced RN care manager leads the team and is responsible for mentoring, making patient rounds and assignments, and making intra-shift adjustments based on real-time patient needs. The RN care manager provides oversight as needed, especially during the initial assessment and discharge planning process as well as providing direct patient care. The RN or LVN care provider provides direct patient care and helps mentor the CA. And the CA completes basic nursing tasks and assists the other team members.
Seton began training and implementation for the first unit adopting the Primary Care Team in 2000. Each new unit took approximately nine months to implement the model. Two of the original designers of the Primary Care Team model oversaw all the initial units during their implementation of the model. They provided developed tools to help with education on the model, provided the education themselves, and provided onsite support. Part of that support included mentoring unit leadership in change management, as many of the unit managers and charge nurses were new to their roles. Recognizing, coping with and supporting staff as they demonstrated the normal behaviors of a major change was some of the most important work done during the implementation. Unless the new model creates benefits that individuals truly value and want for themselves, the status quo is overwhelmingly favored, especially when things get hectic and chaotically busy. Leadership had to learn that this is a common tendency when trying to change a culture, and how to support their staff to recognize the value of the change and establish the new culture in spite of difficult moments and challenges.
The value of the new care model had to be kept in front of staff constantly – patient safety, patient centeredness, support for new nurses, reduced turnover. In addition, very simple measures were tracked prior to and after implementation to show staff the positive changes that were coming about with the care model.
Results of this model
- Patients’ safety and quality outcomes. The implementation of the Primary Care Team model has been correlated with decreases in mortality rates and decreases in the occurrence of pressure ulcers. In addition, one maternity unit experienced an impressive reduction in errors as a result of implementing the Primary Care Team; during the six months following implementation of the model, medication errors dropped 77 percent compared to the six months prior to implementation. After the implementation of the care model on one unit, un-witnessed falls decreased by half for three months in a row. In addition, on some units, both physicians and managers noticed professional growth and improvement in critical thinking skills in the nurses.
- Provider Satisfaction and Retention. Anecdotally, team members and physicians on units that have implemented the Primary Care Team have been satisfied with the new model, especially with team effectiveness. New nurses expressed relief that they received assigned support in the person of the RN Care Manager, and were not “out there alone” in the unit. Nursing students expressed a higher confidence working in units due to being connected to a team with oversight from an experienced nurse. A high number of traveling nurses convert to permanent staff due to the support they receive from the Primary Care Team.
- Patient and Family Satisfaction. Anecdotally, patients and families have repeatedly expressed satisfaction with the care they receive from the Primary Care Team. One specific comment heard repeatedly in the informal narrative surveys was that the call lights were answered so promptly. Other patients expressed surprise when asked, “What is the most important thing we can do for you this shift?” Many stated they had never been asked that question before. Patients’ families expressed their satisfaction with having the nurse’s name on the white board – it helped them know who to ask for if they needed information. Even the physicians appreciated that piece, as they sometimes did not know which nurse had assumed care of their patients unless they saw the name on the board.
HYBRID MODEL
Why is it important to discuss about hybrid model? As we know that there are so many variation exists of nursing care models, and it still cannot answer the nursing issues currently, such as nursing shortage increased, the number of new nurses, different background of nurses, the number of staff, and cost of delivery services. In this chapter, it will discuss about hybrid which is a combination between two or more models, and hope it could be the innovation which is able to answer these issues. However, whatever nursing models are taking places; it should have the best outcome consisting of patient’s satisfaction, nurse satisfaction, quality of care increased, and costly effective.
Rogers (2003) proposed that an innovation is an idea, a practice or objective perceived as new by an individual, a group, or organization. Diffusion is a process of social change in which an innovation is communicated over time through certain channels (mass media or interpersonal) among members of a social system. An individual’s decision to adopt or reject an innovation is conceptualized in several stages. He/she begins with an awareness of an innovation and then forms an attitude toward it based on his/her perception of the innovation (its characteristics). The individual next decides to either adopt or reject the innovation, then implements it, and, finally, confirms his/her decision. The perceived characteristics of an innovation include its relative advantage, compatibility, complexity, trialability, and observability (Rogers, 2003).
According to Rogers (2003), perceived attributes are an innovation’s characteristics that make it more or less appealing to the individual. Relative advantage is the degree to which an innovation is perceived as better than the current idea or practice; the greater the perceived relative advantage of an innovation, the more rapid its rate of adoption. Compatibility is the degree to which an innovation is perceived as consistent with the individual’s existing values, beliefs, past experiences, and needs. Complexity is the degree to which an innovation is perceived as difficult to understand or use. Trialability refers to the degree to which users can alter or implement an innovation on a small scale. Observability is the degree to which the results of an innovation are visible to others. Innovations whose outcomes are easily observed tend to be adopted faster than those with more subtle outcomes (Rogers, 2003).
In this study, the chapter only discusses the first (knowledge) and second (persuasion) stage. It has been no researches are running in this hybrid model. Therefore, it only creates the idea or innovation from situational analysis and previous experience, and will include innovation’s characteristic. The study outline in this chapter is hybrid models which are appropriate to hospital setting, especially in inpatient ward. The previous experiences and situational analysis indicates that many nurses complaint that workforce in inpatient ward is much heavier than other wards. So, the study outline consists of:
- Hybrid: Team and Primary Nursing Model
- Hybrid: Functional and Team Nursing Model
- Hybrid: Case Management and Primary Nursing Model
Hybrid: Team and Primary Nursing Model
To hybrid team and primary nursing model, we have to know firstly the advantage and disadvantage between two models. It might be good combination or not (it is shown in the table below). However, this combination has already applied in Indonesia, and called Professional Nursing Practice Model.
Hybrid: Team and Primary nursing (Professional Practice model)
| Team Nursing | Primary Nursing |
Advantages
|
Advantages
|
Disadvantages
|
Disadvantages
|
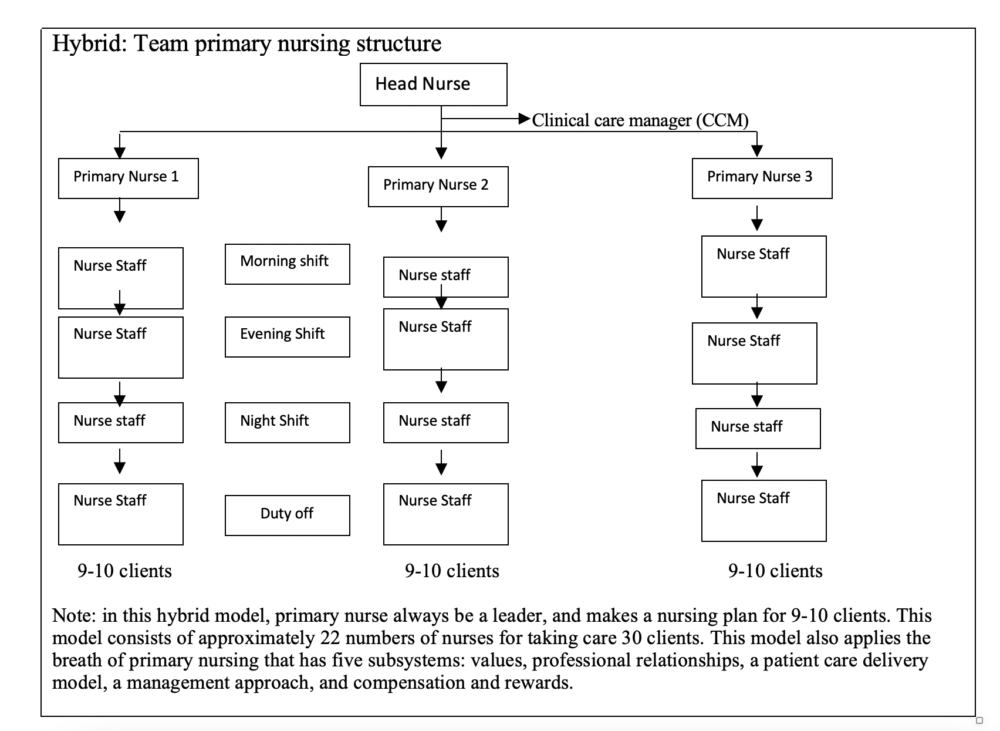
Job Description:
Job and responsibilities of head nurse:
- To arrange shift schedule
- To arrange and control cleanliness and order of ward
- To discuss with staff to solve problem in ward
- To guide students (collaborate with clinical instructor) in implementing nursing care plan, following existing model system
- To do administration
- To do orientation new staff, resident, medical and nursing students who want to practice in ward
- To create and maintain a good relationship with family/client, other health team member
- To develop primary nurse and associate nurse in implementing this model including attitude of professionalism
- If primary nurse in one team is day off, the job and responsibility can be delegated to senior primary nurse, but under the supervision of head nurse and CCM
- To plan and facilitate instrument needed
- To supervise and evaluate the performances of all staffs
- To make routine meeting every month with all nurse staffs in ward to discuss needs
- To plan and evaluate to quality of nursing plan with CCM
- To make a risk map in ward
Job and responsibilities of Clinical Care Manager:
A clinical care manager is a specialized register nurse.
- To guide primary nurse in implementation of this model: validate every diagnosis that primary nurse has already applied, analyze data clients based on documentation, or CCM assesses directly to patients
- Based on validation, give the input to primary nurse, including a reward
- If on client documentation, it is no nursing care plan has been evaluated by primary nurse, so with PN to set diagnose based on client condition and using nursing care standard
- To discuss with primary nurse about division of tasks to associate nurses
- To observe and guide primary nurse related to guidance of PN to associate nurse
- To give input in case discussion of primary nurse to associate nurse
- To present new issues related to nursing care plan
- To identify fact and findings which need evidence
- To identify research problem, set the proposal, and do a research
- To collaborate with head nurse in evaluation of nursing care, coordination, direction, and coordination of students, discuss and evaluation this model
- To set scientific meeting to discuss findings of research about nursing care
Job and responsibilities of Primary Nurse:
A primary nurse is a registered nurse with minimal experience 1 year
- To make a contract with client/family from admission and make a trust relationship
- To do assessment to new client or complete the assessment of primary nurse in other shifts
- To set nursing care plan based on analysis of nursing care standard which fits on assessment
- To explain nursing care plan to associate nurse under the responsibility of their patients in pre-conference
- To set associate nurse who responsible to every client on every shift. Client division is based o the number of clients, level of dependency. If in one shift, PN is accompanied by two associate nurses, so every client is divided to two AN. If PN is only accompanied by one AN in one shift, the number of clients who will be primary nurse responsibility are only 20% which minimal level of dependency. This rule for primary nurse to have a time in guiding and helping associate nurse in implementing nursing care
- To guide and evaluate associate nurse in doing nursing action, based on standard or not
- To monitor documentation of associate nurse
- To help and facilitate associate nurse activity
- To do nurse action that associate nurse cannot do
- To arrange the implementation of the consul and laboratory
- To do nursing round under primary nurse responsibility
- To accompany doctor visit. If there is no primary nurse, it will be accompanied by associate nurse
- To evaluate nursing care and make a progress note every day
- To conduct meeting with family or patient minimal every two days to discuss client condition (depends on client condition)
- If PN is duty off, the jobs of PN will be delegated to associate nurse with guidance of head nurse or CCM
- To do health education to family and client
- To make a discharge planning
- To collaborate with CCM in identifying issue needed evidence in order to make evidence-based practice
Job description and responsibilities of Associate Nurse:
Associate nurse is Licensed practice nurse (LPN), technical nurse, register nurse, nurse diploma.
- To read nursing care plan which has already set by primary nurse
- To develop therapeutic relationship with client/family, which is an extension contract of primary nurse
- To accept new client and give the information based on orientation format of client and family, if PN is not exist
- To implement nursing care-based nursing care plan
- To evaluate the action having been done and document it in available format
- To follow visit doctor, if primary nurse is not existing
- To check nursing status
- To make a report of schedule changing
- To prepare client to diagnostic check, laboratory, treatment, and action.
- To do facilitation inventory related to the team
- To help another team
How to implement or apply this model?
|
Days to |
Classification | Number of clients | Number of nurses | information | ||||
| Min | Partial | Total | Morning | Evening | night | |||
| 1 | 12 | 9 | 6 | 27 | 6.63 | 4.83 | 3.30 | |
| 2 | 14 | 8 | 3 | 25 | 5.62 | 3.06 | 2.56 | |
| 22 | 9 | 12 | 7 | 28 | 7.29 | 5.16 | 3.15 | |
| Average | 7.11 | 5.28 |
3.35 |
|||||
Preparation phase
- Make one team work
- Score to the quality of nursing care in your hospital currently
- Present this model and result of quality care of model applied in your hospital to hospital and nurse manager
- Set the ward/ room to implement the model
- Identify the number of clients in 7 days based on level of dependency. Determine the number of nurses needed by using Douglas formula in 22 days. Calculation of the number of nurses based on Level of Dependency (LOD) Douglas formula 1984. For trying this model, calculation of nurse in 22 days (4 weeks).
- Make a deal of primary nurse and associate nurse criteria (PPM 1, PPM 2, PPM 3)
- Develop standard of nursing care plan for several main cases in every in patient room
- Set up documentation format
Example in 22 days:
12 x 0.17 = 2.04
9 x 0.27 = 2.43
6 x 0.36 = 2.16
Total 6.63 = 6 nurses
7.11 + 5.28 + 3.35 = 15.75 = 16 nurses + 5 nurses (day off)
16+ 5 = 21 nurse + 1 head nurse + 3 primary nurses = 25 nurses for 26-30 clients
Implementation Phase
- Train primary nurse and associate nurse
- Guide primary nurse when doing pre-post conference, case study, and about nurse documentation
| Number of clients | Client classification | ||||||||
| Minimum | Partial | Total | |||||||
| Morning | Evening | Night | Morning | Evening | Night | Morning | Evening | Night | |
| 1 | 0.17 | 0.14 | 0.07 | 0.27 | 0.15 | 0.10 | 0.36 | 0.30 | 0.20 |
| 2 | 0.34 | 0.28 | 0.14 | 0.54 | 0.30 | 0.20 | 0.72 | 0.60 | 0.40 |
| 3 | 0.51 | 0.42 | 0.21 | 0.81 | 0.45 | 0.30 | 1.08 | 0.90 | 0.60 |
| Cont. | |||||||||
Evaluation Phase
- Evaluate the quality of nursing care
- Identify factors influencing the result
Innovation Characteristic Perceived by Rogers’ Model to Team Primary Nursing Model
| Innovation Characteristic | Themes in Team Primary Nursing Model |
| Relative advantage |
|
| Compatibility |
|
| Complexity |
|
| Trialability |
|
| Observability |
|
Hybrid: Functional and Team Nursing Model
As the same as first step to hybrid two models, we have to see the advantages and disadvantages between two models
| Functional model | Team nursing model |
Advantages
|
Advantages
|
Disadvantages
|
Disadvantages
|
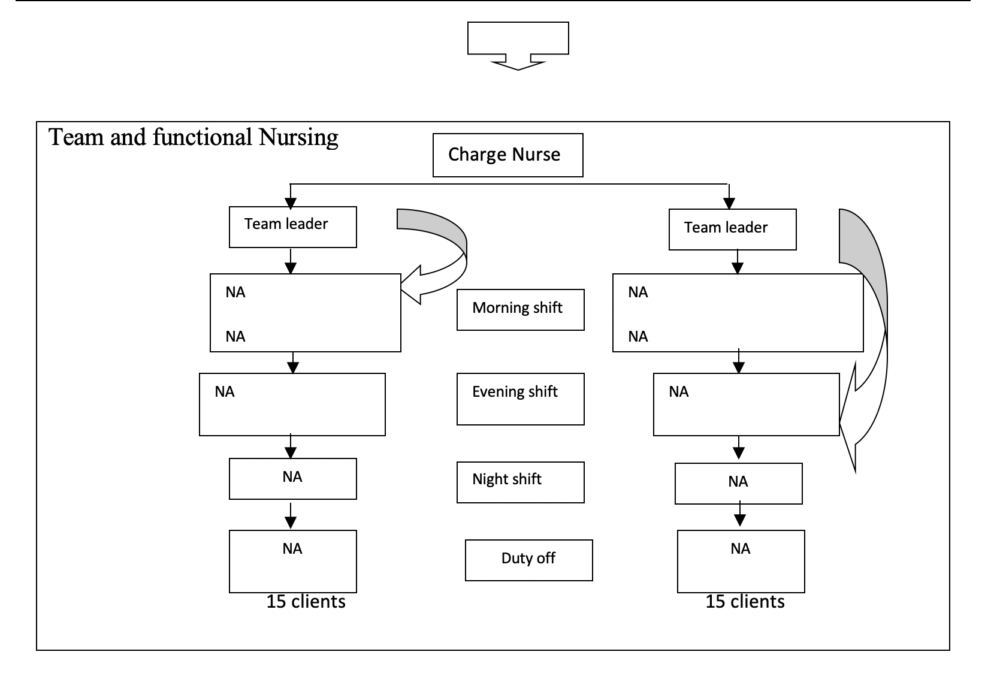
Innovation Characteristic Perceived by Rogers’ Model to Functional and Team Nursing Model
| Innovation Characteristic | Themes in Team Primary Nursing Model |
| Relative advantage |
|
| Compatibility |
|
| Complexity |
|
| Trialability |
|
| Observability |
|
To see the combination structure between team, primary, and functional model
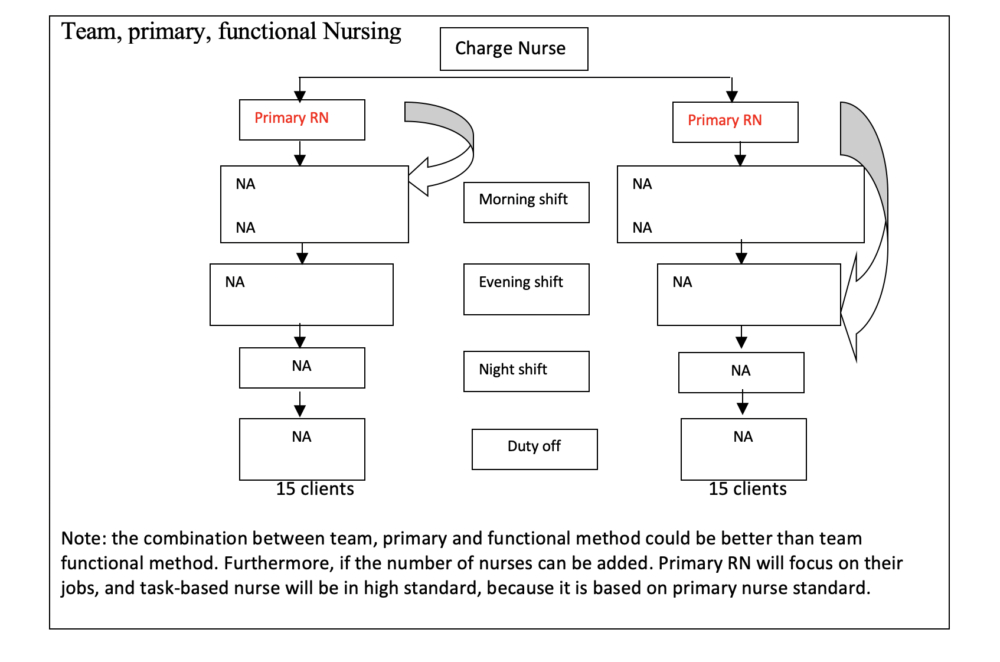
Hybrid: Case management and primary nursing model
As the first and second hybrid, we have to see the advantages and disadvantages between two models. Case management and primary nursing are almost the same. It means a professional has a responsibility to coordinate care to one client. The difference is Case management coordinates care in multidisciplinary and its focus on planning, coordination, and care evaluation. Whereas, in Primary Nursing, primary nurse coordinate and implemented nursing care to client from admission till discharge or move to another ward. Combination between two models will be holistic in not only economic factor by decrease length of stay, but also the quality of care by using the breath of primary nursing. Finally, it will absolutely have an effect to best patient and nurse satisfaction.
| Case Management | Primary Nursing |
Advantages
|
Advantages
|
Disadvantages
|
Disadvantages
|
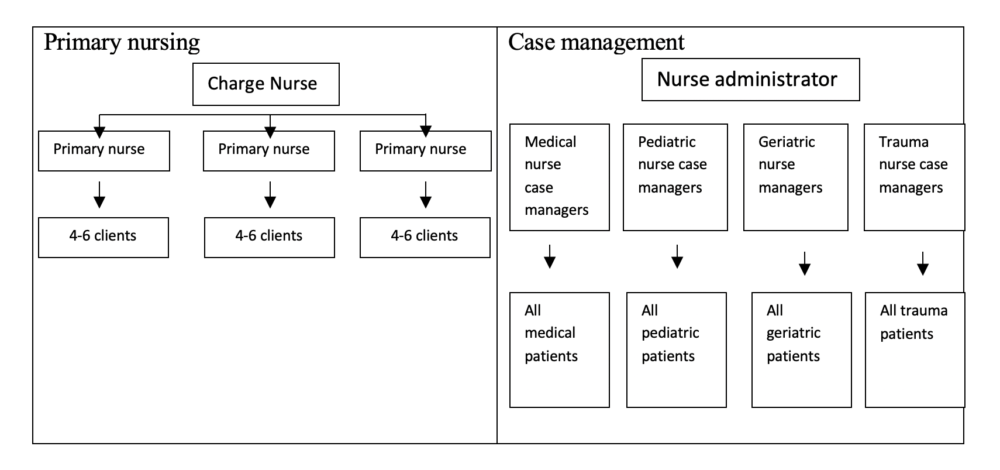
Innovation Characteristic Perceived by Rogers’ Model to case management primary nursing Model
| Innovation Characteristic | Themes in Team Primary Nursing Model |
| Relative advantage |
|
| Compatibility |
|
| Complexity |
|
| Trialability |
|
| Observability |
|
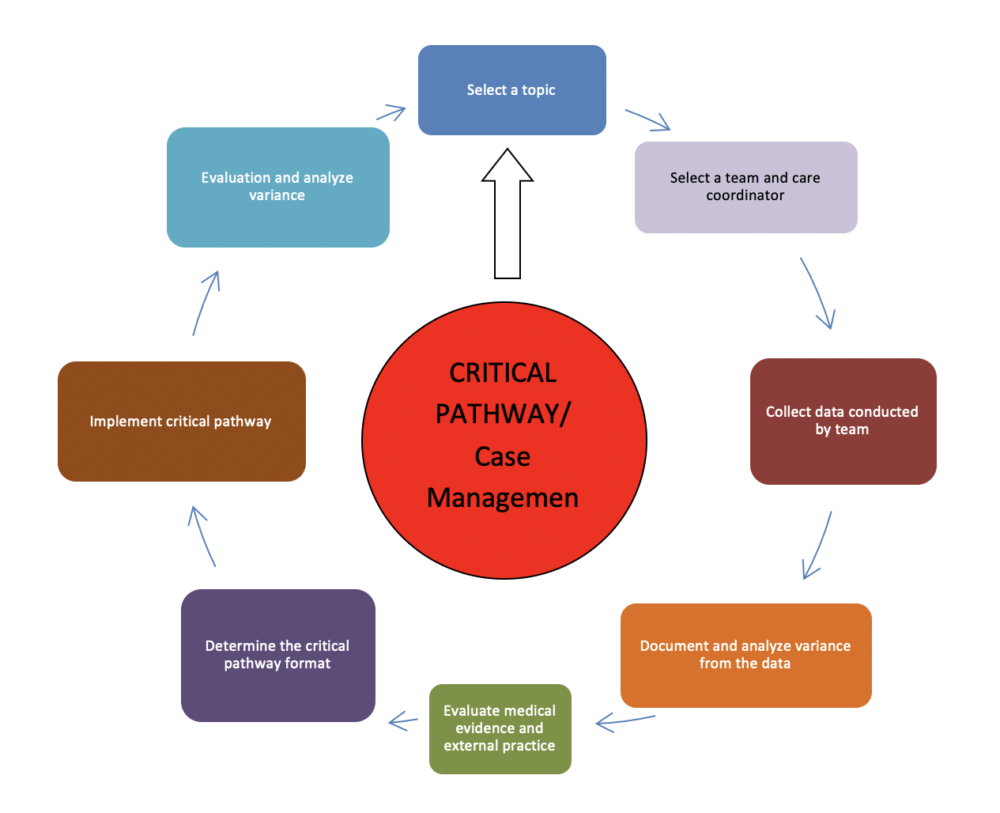
Steps in critical pathway
There are following steps to implement this model, especially critical pathway in case management:
Summary
Hybrid models are a solution to answer the variation of nursing model delivery. This model is going to improve quality of care and outcome. However, it depends on the organizational resources, patient population, and talent on the staff.
Based on three hybrids above, it can be concluded the steps in doing the hybrid model. The following steps are:
- Make one teamwork
- Critic and analyze the problem or score the quality of nursing care in your hospital
- Identify the number of client based on level of dependency or patient classification
- Determine the number of nurses as needed
- Determine the hybrid model to use (see the outcome; advantages and disadvantages, benefit for patient and nurse, cost effectiveness and sustainability)
- Find the research to support
- Implementation
- Evaluation (to measure the quality of your hybrid nursing model)
Limitation of this paper
Because there is no research to support these hybrid models, it is difficult to provide cost of innovation, indicator to measure outcome. The findings are only based on situational analysis and previous experience, it might be not representative the data analysis. However, the author believes that these hybrids models could solve the nurse problem, especially in hospital setting.
References
AACN, Acute Care Nurse Practitioner (ACNPC™) Test Plan
Hoffart, N., Woods, Q.C. (1996). Elements of a Nursing Professional Practice Model. Journal of Professional Nursing. Vol 12. No 26: pp 354-364
Innovative Care Models. Retrieved at: http://www.innovativecaremodels.com
Jennifer, J., Kimball, B. (2008). Innovative Care Delivery Models: Identifying New Models that Effectively Leverage Nurses.
Leadership in Nursing Practice: Nursing Care Delivery System. University of North Carolina at Chapel Hill School of Nursing
Mascarenhas, K. (2001). Patient Satisfaction with the Comprehensive Care Model of Dental Care Delivery
Sitorus, R. (2006). Model Praktek Keperawatan Professional di Rumah Sakit; Penataan Struktur dan Proses (Sistem) Pemberian Asuhan Keperawatan di Ruang Rawat. Cetakan I. Penerbit Buku Kedokteran: EGC.